药品详情:
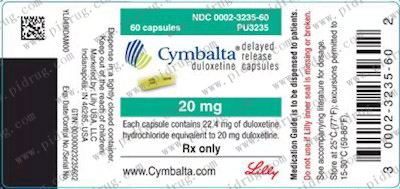
【功能与主治】欣百达Cymbalta用于治疗抑郁症。
【型号与规格】 铝塑泡罩包装,14粒/盒
【用法与用量】起始治疗:推荐本品的起始剂量为40mg/日(20mg一日二次)至60mg/日(一日一次或30mg一日二次),不考虑进食情况。现有的临床研究数据未证实剂量超过60mg/日将增加疗效。
维持/继续/长期治疗:一般认为抑郁症的急性发作需要数月或更长时间的药物治疗,但尚没有充足的试验资料来确定患者应该连续服用度洛西汀治疗达多长时间。对此类患者,应对其接受维持治疗的必要性以及相应所需的剂量作定期评估。
特殊人群:肾脏功能受损患者的用量一对于晚期肾脏疾病(需要透析的)患者,或有严重肾脏功能损害(估计肌酐清除率<30 mL/min的)患者,建议不用本品(见药理毒理)。
肝功能不全的患者的用量一建议有任何肝功能不全的患者避免服用本品(见药理毒理和注意事项)
老年患者的用量一对于老年患者,建议不必根据年龄调整剂量。与任何药物一样,治疗老年患者时应该慎重。在老年患者中个体化调整剂量时,增加剂量时应该额外小心。
对妊娠后三个月的女性患者的治疗一在妊娠后三个月内接触SSRIs或SNRls(五羟色胺和去甲肾上腺素再摄取抑制剂)的新生儿,产生的并发症会导致住院时间延长、需要呼吸支持和管道喂食(见注意事项)。当孕期女性用度洛西汀治疗时,在妊娠后三个月,医生应对治疗的潜在风险和获益进行认真的评价。医生应考虑在妊娠晚期逐渐减度洛西汀的用量。
已有报道本品及其他SSRI和SNRIs药物的停药反应(见注意事项)。停药时应对这些症状进行监测。建议尽可能的逐渐减药,而不是骤停药物。由于减少药物剂量或停药而引起了无法耐受的症状时,可以考虑恢夏使用以往的的处方剂量。随后再以更慢的的速度减药。
MOAT停药后至少14天才可开始本品的治疗。本品停药后至少5天才可以开始MOAT的治疗(见禁忌和警告)。
【注意事项】肝脏毒性一度洛西汀有增加血清转氨酶水平的风险。肝脏转氨酶升高导致0.4%(31/8454)度洛西汀治疗的患者中断治疗。这些患者出现转氨酶升高的时间中位数为2个月。在抑郁症患者中进行的对照试验中,0.9%(8/930)用度洛西汀治疗的患者ALT升高超过正常上限3倍以上,而安慰剂组中为0.3%(2/652)。所有安慰剂对照研究中,度洛西汀组中有1%(39/3732)的患者ALT升高超过正常上限3倍以上,而安慰剂组中为0.2%(6/2568)。固定剂量的安慰剂对照研究中,有证据显示ALT升高超过正常上限3倍和AST升高超过正常上限5倍,与药物剂量有量效关系。上市后监测还报道出现腹痛、肝肿大、伴有或无黄疽的转氨酶升高超过正常值上限20倍的肝炎病例,反映了混合性或肝细胞性损伤,也有出现转氨酶无明显升高的胆汁郁积型黄疽病例的报道。
在排除梗阻的情况下,通常认为转氨酶升高伴有胆红素升高,是严重肝脏损害的重要指标。国外临床试验中,3名服用度洛西汀的患者,出现转氨酶、胆红素和碱性磷酸酶升高,提示存在梗阻情况。上述患者有严重的过度饮酒的情况,这可能是出现上述异常指标的原因所在。两名安慰剂治疗的患者也出现了转氨酶、胆红素升高的情况。上市后报告显示转氨酶、胆红素和碱性磷酸酶升高也可以发生在患有慢性肝病或肝硬化患者中。因为度洛西汀和酒精的相互作用可能引起肝损害或者加剧已有的肝病恶化,所以度洛西汀通常不用于有习惯性饮酒和慢胜肝病患者的治疗。对血压的影响一与安慰剂相比,度洛西汀治疗引起血压升高,平均升高:收缩压2 mm Hg,舒张压0.5 mm Hg,偶尔有至少一次测量的收缩压大于140 mmHg。
治疗开始前应测量血压,治疗后应定期测量。(见不良反应,生命体征变化)转为躁狂/轻躁狂一在MDD安慰剂对照试验中,据报导,度洛西汀组中有0.1%(1/1139)的患者转为躁狂/轻躁狂,安慰剂组为0.1%(1/777)。据报导,用其他已经上市对MDD有效药物治疗的一小部分患者转为躁狂/轻躁狂。因此,与其他抗抑郁药一样,既往有躁狂史的患者慎用度洛西汀。癫痫-还未系统评价度洛西汀在癫痫障碍患者中的疗效。这些患者从临床试验中排除了。在抑郁症患者的安慰剂对照临床试验中,度洛西汀组中有0.1%(1/1139)的患者出现癫痫发作,而安慰剂组为0%(0/777)。既往有癫痫发作史的患者慎用度洛西汀治疗已得到控制的窄角性青光眼-临床试验显示,度洛西汀有增加瞳孔散大的风险。
因此,度洛西汀慎用于已稳定的窄角性青光眼患者(见禁忌,禁用未经治疗的闭角性青光眼)。停药-已对度洛西汀的停药症状做过系统研究。在抑郁症患者中进行的为期9周的安慰剂对照试验中,骤停药物,观察到度洛西汀治疗的患者发生率2%或明显高于骤停安慰剂的症状,包括:头晕、恶心、头痛、感觉异常、呕吐、易怒、噩其他SSRIs和SNRIs上市以来,经常报道因为停用上述药物引起的不良反应,尤其是骤停药物后出现的,包括恶劣心境、易怒、兴奋、头晕,感觉紊乱(感觉异常和电击感),焦虑、意识模糊、头痛、情感脆弱、乏力、失眠、轻躁狂、耳鸣、癫痫等等。虽然上述不良反应有自限性,但有些很严重。
停药度洛西汀后应注意观察患者有无上述症状的出现。建议尽可能的逐渐减药,而不是骤停药物。由于减少药物剂量或停药而引起了无法耐受的症状时,可以考虑应用以往的处方剂量。然后,临床医生再以一个更慢的速度减药。(见用法用量)。
患者合并躯体疾病-度洛西汀治疗合并躯体疾病患者的临床经验有限。尚无胃动力改变对度洛西汀肠溶包衣的稳定性影响的资料。由于度洛西汀在酸性媒介中迅速水解成萘酚,有胃排空减缓的患者注意避免使用度洛西汀(如一些糖尿病患者)。
度洛西汀还未在近期有心肌梗塞或不稳定性冠状动脉动脉疾病患者中进行系统评估。药物上市前的临床研究中,上述患者常作为排除者,未能进入研究中。不过,在MDD安慰剂对照试验中,321名服度洛西汀患者的心电图与基线时正常心电图比较,度洛西汀不会增加有临床意义的心电图异常(见不良反应,心电图改变)。
终末期肾病(需要透析)和严重肾功能不全(Cr清除率<30ml/min)患者使用度洛西汀其血药浓度会增加,尤其是它的代谢产物。因此,不推荐终末期肾病患者使用度洛西汀(见药理毒理和用法用量)。
肝功能不全患者使用度洛西汀其血药浓度会明显增加,因此不推荐此类患者服用度洛西汀(见药理毒理和用法用量)。
【不良反应及禁忌】MDD急性期治疗的安慰剂对照研究中,接受度洛西汀治疗的患者中,发生率≧2%以及高于安慰剂组的不良反应。其中最常见的不良反应(发生率≧5%,且至少是安慰剂组发生率的两倍)包括恶心、口干、便秘、食欲下降、疲乏、嗜睡、出汗增多(详情请咨询专科医生)
尿急-度洛西汀属于已知的影响尿道阻力的药物。如果应用度洛西汀治疗的过程中出现尿急,应当考虑药物导致的可能性。
实验室变化-9周MDD或13周DPNP安慰剂对照研究中,与基线比较,度洛西汀治疗结束后,ALT、AST、CPK和碱性磷酸(醋)酶均值出现轻度增高。与安慰剂组比较,度洛西汀治疗的患者中出现这些异常值表现为偶发、中度、一过性的异常(见注意事项)。
生命体征改变-在为期9周的MDD安慰剂对照研究中,度洛西汀的剂量为40-120mg/日,导致血压升高,与安慰剂比较,收缩压平均升高2mrnHg,舒张压平均升高0.5mmHg,收缩压超过140mmHg的发生率增加。
9周的MDD和13周DPN尸安慰剂对照研究中,度洛西汀治疗导致心率轻度增加,与安慰剂比较约增加2次/分钟。
体重变化-在MDD安慰剂对照研究中,应用度洛西汀治疗9周的患者体重平均下降约0.5kg,而安慰剂治疗的患者体重平均增加约0.2kg。
在糖尿病周围神经痛的安慰剂对照临床试验中,接受度洛西汀治疗13周的患者平均体重降低约1.1kg,安慰剂治疗的患者体重平均增加约0.2kg。
心电图的改变-持续8周的MDD安慰剂对照研究中,321例度洛西汀治疗和169例安慰剂治疗的患者进行了心电图检查。心率校正后的QT(QTc)间期在度洛西汀和安慰剂治疗的患者之间没有差异。两者之间在QT、PR、QRS间期之间无显著差异。
在为期13周的DPNP安慰剂对照研究中,528例接受度洛西汀治疗和205例安慰剂治疗的患者进行了心电图检查。接受度洛西汀治疗的患者,其心率校正后的QT《QTc》间期改变与安慰剂治疗者无差异。度洛西汀治疗组和安慰剂治疗组的QT、PR、QRS或QTc间期检查均未发现有临床意义的显著差异。
上市前度洛西汀治疗抑郁症出现的其它不良反应(见原装说明书描述)
【禁忌】过敏度洛西汀肠溶胶囊禁用于已知对度洛西汀肠溶胶囊或产品中任何非活性成分过敏的患者。
【孕妇用药】对妊娠后三个月的女性患者的治疗一在妊娠后三个月内接触SSRIs或SNRls(五羟色胺和去甲肾上腺素再摄取抑制剂)的新生儿,产生的并发症会导致住院时间延长、需要呼吸支持和管道喂食(见注意事项)。当孕期女性用度洛西汀治疗时,在妊娠后三个月,医生应对治疗的潜在风险和获益进行认真的评价。医生应考虑在妊娠晚期逐渐减度洛西汀的用量。
【儿童用药】对于儿童患者的疗效和安全性尚不清楚(见警告)。如果考虑在儿童青少年中使用度洛西汀,必须权衡潜在的风险和临床需要。
【贮藏】 15一30℃室温保存
Cymbalta(Duloxetine)
Duloxetine, sold under the brand name Cymbalta among others,[1] is a medication used to treat major depressive disorder, generalized anxiety disorder, fibromyalgia, and neuropathic pain.[2] It is taken by mouth.[2]
Common side effects include dry mouth, nausea, feeling tired, dizziness, agitation, sexual problems, and increased sweating.[2] Severe side effects include an increased risk of suicide, serotonin syndrome, mania, and liver problems.[2] Antidepressant withdrawal syndrome may occur if stopped.[2] There are concerns that use during the later part of pregnancy can harm the baby.[2] It is a serotonin–norepinephrine reuptake inhibitor.[3] How it works is not entirely clear.[2]
Duloxetine was approved for medical use in the United States in 2004.[2] It is available as a generic medication.[3] In the United States the wholesale cost per dose is about 0.20 USD as of 2018.[4] In 2016 it was the 48th most prescribed medication in the United States with more than 15 million prescriptions.[5]
Medical uses
The main uses of duloxetine are in major depressive disorder, generalized anxiety disorder, neuropathic pain, chronic musculoskeletal pain, and fibromyalgia.
Duloxetine is recommended as a first line agent for the treatment of chemotherapy-induced neuropathy by the American Society of Clinical Oncology,[9] as a first-line therapy for fibromyalgia in the presence of mood disorders by the German Interdisciplinary Association for Pain Therapy,[10] as a Grade B recommendation for the treatment of diabetic neuropathy by the American Association for Neurology[11] and as a level A recommendation in certain neuropathic states by the European Federation of Neurological Societies.[12]
A 2014 Cochrane review concluded that duloxetine is beneficial in the treatment of diabetic neuropathy and fibromyalgia but that more comparative studies with other medicines are needed.[13] The French medical journal Prescrire concluded that duloxetine is no better than other available agents and has a greater risk of side effects.[14] Thus they recommend against its general use.[14]
Major depressive disorder
Duloxetine was approved for the treatment of major depression in 2004. While duloxetine has demonstrated improvement in depression-related symptoms compared to placebo, comparisons of duloxetine to other antidepressant medications have been less successful. A 2012 Cochrane Review did not find greater efficacy of duloxetine compared to SSRIs and newer antidepressants. Additionally, the review found evidence that duloxetine has increased side effects and reduced tolerability compared to other antidepressants. It thus did not recommend duloxetine as a first line treatment for major depressive disorder, given the (then) high cost of duloxetine compared to inexpensive off-patent antidepressants and lack of increased efficacy.[15] Generic duloxetine became available in 2013.[16]
Generalized anxiety disorder
Duloxetine is more effective than placebo in the treatment of generalized anxiety disorder(GAD).[17] Major guidelines such as Maudsley Prescribing Guidelines,[18] and Canadian Psychiatric Association Guidelines[19] do not list duloxetine among the recommended treatment options. A review from the Annals of Internal Medicine lists duloxetine among the first line drug treatments, however, along with citalopram, escitalopram, sertraline, paroxetine, and venlafaxine.[20]
Diabetic neuropathy
Duloxetine was approved for the pain associated with diabetic peripheral neuropathy (DPN), based on the positive results of two clinical trials. The average daily pain was measured using an 11-point scale, and duloxetine treatment resulted in an additional 1–1.7 points decrease of pain as compared with placebo.At least 50% pain relief was achieved in 40–45% of the duloxetine patients vs. 20–22% of placebo patients. Pain decreased by more than 90%, in 9–14% of duloxetine patients vs. 2–4% of placebo patients. Most of the response was achieved in the first two weeks on the medication. Duloxetine slightly increased the fasting serum glucose; this effect was deemed to be of "minimal clinical significance", however.
The comparative efficacy of duloxetine and established pain-relief medications for DPN is unclear. A systematic review noted that tricyclic antidepressants (imipramine and amitriptyline), traditional anticonvulsants and opioids have better efficacy than duloxetine. Duloxetine, tricyclic antidepressants and anticonvulsants have similar tolerability while the opioids caused more side effects.[24] Another review in Prescrire International considered the moderate pain relief achieved with duloxetine to be clinically insignificant and the results of the clinical trials unconvincing. The reviewer saw no reason to prescribe duloxetine in practice.[25] The comparative data collected by reviewers in BMC Neurology indicated that amitriptyline, other tricyclic antidepressants and venlafaxine may be more effective. The authors noted that the evidence in favor of duloxetine is much more solid, however.[26] A Cochrane review concluded that the evidence in support of duloxetine's efficacy in treating painful diabetic neuropathy was adequate, and that further trials should focus on comparisons with other medications.[13]
Fibromyalgia and chronic pain
A review of duloxetine found that it reduced pain and fatigue, and improved physical and mental performance compared to placebo.
The U.S. Food and Drug Administration (FDA) regulators approved the drug for the treatment of fibromyalgia in June 2008.
It may be useful for chronic pain from osteoarthritis.
On November 4, 2010, the U.S. Food and Drug Administration approved duloxetine to treat chronic musculoskeletal pain, including discomfort from osteoarthritis and chronic lower back pain.
Stress urinary incontinence
Duloxetine failed to receive US approval for stress urinary incontinence amid concerns over liver toxicity and suicidal events; it was approved for this use in the UK, however, where it is recommended as an add-on medication in stress urinary incontinence instead of surgery.
The safety and utility of duloxetine in the treatment of incontinence has been evaluated in a series of meta analyses and practice guidelines.
§ A 2017 meta-analysis found that harms are at least as great if not greater than the benefits.
§ A 2013 meta-analysis concluded that duloxetine decreased incontinence episodes more than placebo with people about 56% more likely than placebo to experience a 50% decrease in episodes. Adverse effects were experienced by 83% of duloxetine-treated subjects and by 45% of placebo-treated subjects.
§ A 2012 review and practice guideline published by the European Association of Urology concluded that the clinical trial data provides Grade 1a evidence that duloxetine improves but does not cure urinary incontinence, and that it causes a high rate of gastrointestinal side effects (mainly nausea and vomiting) leading to a high rate of treatment discontinuation.[35]
§ The National Institute for Clinical and Health Excellence recommends (as of September 2013) that duloxetine not be routinely offered as first line treatment, and that it only be offered as second line therapy in women wishing to avoid therapy. The guideline further states that women should be counseled regarding the drug's side effects.[36]
Contraindications
The following contraindications are listed by the manufacturer:
§ Hypersensitivity: duloxetine is contraindicated in patients with a known hypersensitivity to duloxetine or any of the inactive ingredients.
§ Monoamine oxidase inhibitors (MAOIs): concomitant use in patients taking MAOIs is contraindicated.
§ Uncontrolled narrow-angle glaucoma: in clinical trials, Cymbalta use was associated with an increased risk of mydriasis (dilation of the pupil); therefore, its use should be avoided in patients with uncontrolled narrow-angle glaucoma, in which mydriasis can cause sudden worsening.
§ Central nervous system (CNS) acting drugs: given the primary CNS effects of duloxetine, it should be used with caution when it is taken in combination with or substituted for other centrally acting drugs, including those with a similar mechanism of action.
§ Duloxetine and thioridazine should not be co-administered.
In addition, the FDA has reported on life-threatening drug interactions that may be possible when co-administered with triptans and other drugs acting on serotonin pathways leading to increased risk for serotonin syndrome.[38]
Adverse effects
Nausea, somnolence, insomnia, and dizziness are the main side effects, reported by about 10% to 20% of patients.[39]
In a trial for major depressive disorder (MDD), the most commonly reported treatment-emergent adverse events among duloxetine-treated patients were nausea (34.7%), dry mouth (22.7%), headache (20.0%) and dizziness (18.7%), and except for headache, these were reported significantly more often than in the placebo group.[40] In a long-term study of fibromyalgia patients receiving duloxetine, frequency and type of adverse effects was similar to that reported in the MDD above. Side effects tended to be mild-to-moderate, and tended to decrease in intensity over time.
In 4 clinical trials of duloxetine for the treatment of MDD, sexual dysfunction occurred significantly more frequently in patients treated with duloxetine than those treated with placebo, and this difference occurred only in men.Specifically, common side effects include difficulty becoming aroused, lack of interest in sex, and anorgasmia (trouble achieving orgasm). Loss of or decreased response to sexual stimuli and ejaculatory anhedonia are also reported. Frequency of treatment-emergent sexual dysfunction were similar for duloxetine and SSRIs when compared in a 6 month observational study in depressed patients.Rates of sexual dysfunction in MDD patients treated with duloxetine vs escitalopram did not differ significantly at 4, 8, and 12 weeks of treatment, although the trend favored duloxetine (33.3% of duloxetine patients experienced sexual side effects compared to 43.6% of those receiving escitalopram and 25% of those receiving placebo).
Mechanism of action
|
Binding profile[52] |
|
Receptor |
Ki (nM) |
|
SERT |
0.8 |
|
NET |
7.5 |
|
DAT |
240 |
|
5-HT2A |
504 |
|
5-HT2C |
916 |
|
5-HT6 |
419 |
Duloxetine inhibits the reuptake of serotonin and norepinephrine (NE) in the central nervous system. Duloxetine increases dopamine (DA) specifically in the prefrontal cortex, where there are few DA reuptake pumps, via the inhibition of NE reuptake pumps (NET), which is believed to mediate reuptake of DA and NE.[53] Duloxetine has no significant affinity for dopaminergic, cholinergic, histaminergic, opioid, glutamate, and GABA reuptake transporters, however, and can therefore be considered to be a selective reuptake inhibitor at the 5-HT and NE transporters. Duloxetine undergoes extensive metabolism, but the major circulating metabolites do not contribute significantly to the pharmacologic activity.
Major depressive disorder is believed to be due in part to an increase in pro-inflammatory cytokines within the central nervous system. Antidepressants including ones with a similar mechanism of action as duloxetine, i.e. serotonin metabolism inhibition, cause a decrease in proinflammatory cytokine activity and an increase in anti-inflammatory cytokines; this mechanism may apply to duloxetine in its effect on depression but research on cytokines specific to duloxetine therapy is lacking.
The analgesic properties of duloxetine in the treatment of diabetic neuropathy and central pain syndromes such as fibromyalgia are believed to be due to sodium ion channel blockade.
注:药品如有新包装,以新包装为准。以上资讯来源于网络或由高等医药院校的学生志愿者翻译(如有错漏,请帮忙指正),仅供医护人员内部讨论,不作任何用药依据,具体用药指引,请咨询主治医师。
如您发现本网站有文字编辑或内容错误,请点击此处发送(需要安装有foxmail或outlook支持),
或发邮件至:info@pidrug.com,香港济民药业感谢您的到访!
欢迎您添加香港济民药业微信,或在公众号内留言。